Discovering treatments for Alzheimer’s disease
How a Book Is Undermining Progress Against Alzheimer's — Public trust is easily cracked and, once cracked, hard to repair (MedPageToday March 5, 2025).
Aduelm was a mess — and it could happen again (STAT News — February 6, 2024)
The FDA needs a risk evaluation and mitigation strategy for Alzheimer’s drug lecanemab (STAT News — June 16, 2023)
How can the latest Alzheimer’s therapy reach patients? Follow this trustworthy process (STAT News — October 3, 2022)
Restoring Trust in the FDA (Panel Discussion) (The Greenwall Foundation — September 29, 2022)
The Search for a Coherent Language: The Science and Politics of Drug Testing and Approval (Ethics, Law and Aging Review — Vol. 8, 2002)
The Strange Story of Aducanumab
On June 7, 2021, the FDA granted accelerated approval to aducanumab (Aduhelm) for the treatment of Alzheimer disease, the first approval of an Alzheimer’s drug in decades. But Karlawish didn’t celebrate the approval. Biogen’s case was based on questionable science, and yet the FDA approved Aduhelm with an overly broad label. Through a series of academic and public writings, Karlawish warned the FDA against approval, analyzed the controversial decision, and documented the resulting turmoil. In the end, the system worked, freedom worked. Government investigations, free markets, a free press, and open debate in the expert community pushed the drug from the market.
Aducanumab: the beginning of the end of Alzheimer’s disease? (STAT News — December 6, 2019)
Aducanumab isn’t the simple solution to the complicated Alzheimer’s crisis (STAT News — December 20, 2019)
If the FDA approves Biogen’s Alzheimer’s treatment, I won’t prescribe it (STAT News — May 30, 2021)
The Problem of Aducanumab for the Treatment of Alzheimer Disease (Annals of Internal Medicine - June 17, 2021)
"A disease does not fully exist in America until it has a business model" (Audio Essay) (Whiskey & Cream, Episode XX - June 19, 2021)
The approval of Aduhelm risks eroding public trust in Alzheimer research and the FDA (Nature Reviews | Neurology - July 15, 2021)
We can’t drug our way out of despair over Alzheimer’s (The Philadelphia Inquirer — August 6, 2021)
Aducanumab and the Business of Alzheimer Disease — Some Choice (JAMA Neurology — August 19, 2021)
What just happened? The strange tale of the FDA's approval of aducanumab for the treatment of Alzheimer's disease (UPenn Research Ethics and Policy Series — October 4, 2021)
Aduhelm for Alzheimer’s disease: too risky to say yes; too desperate to say no. Medicare has a plan to help patients choose wisely. (Penn Memory Center — February 5, 2022)
Fix the process that led to Alzheimer’s drug fiasco (Nature — May 31, 2022)
Overhyped Alzheimer’s treatments betrayed patients’ hopes. Here’s how science should change (LA Times — June 20, 2022)
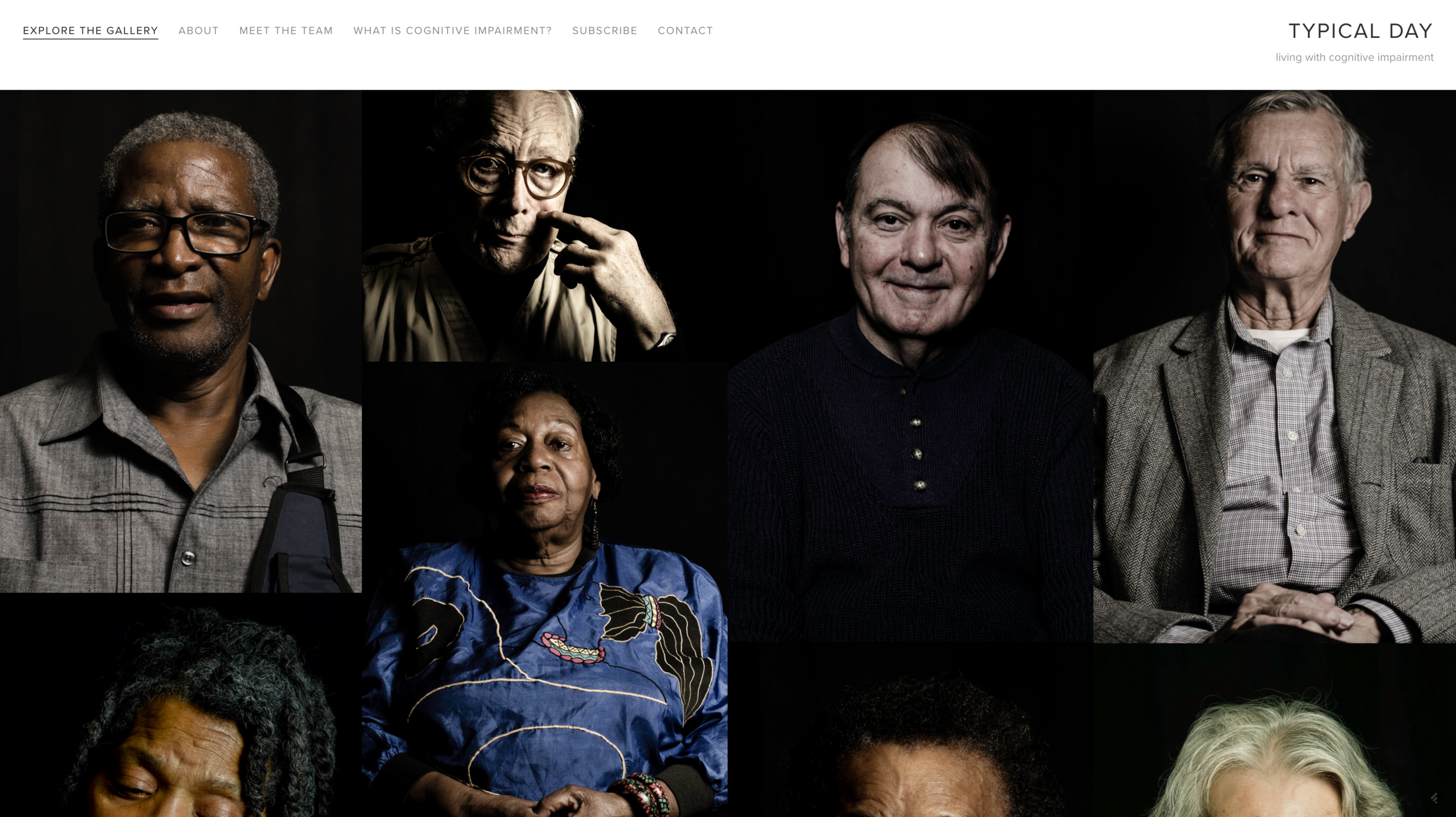
Living with cognitive impairments or the risk of them
All diseases are “bad,” or at least unpleasant. A disease that isn’t ought to prompt serious questioning about why we labeled the set of signs and symptoms a disease. Some diseases are, of course, worse than others, and of all the diseases of aging, Alzheimer’s, and other causes of dementia such as Lewy Body disease stand out as distinctly distressing.
Why?
Over a series of writings, Karlawish has probed narratives of the patient and caregiver experiences, and the mixed fortunes of researchers, clinicians, and policy makers’ efforts to tackle the problem of dementia (he wrote several of these as a columnist for Forbes). One of his conclusions is that early on, and relentlessly, these diseases chip away at a person’s ability to self-determine her life. Alzheimer’s is best thought of as a disease of our autonomy.
This work has also included innovative scholarship to develop novel methods to assess decisional abilities, including the ground-breaking Assessment of Capacity for Everyday Decision-making, or ACED, an instrument that assists a professional in deciding whether a person can solve an everyday functional problem, such as managing mistakes with financial matters.
How can we really live with Alzheimer’s? (The Philadelphia Inquirer — March 8, 2015)
Alzheimer’s Disease Patients Are The Last Casualties Of The Cold War (Forbes — July 30, 2016)
An Alzheimer’s Doctor Reveals His Most Powerful Technology (Forbes — August 5, 2016)
Still More Bad News for Patients with Alzheimer’s Disease, and Now America’s Women (Forbes — July 1, 2017)
Aducanumab isn’t the simple solution to the complicated Alzheimer’s crisis (STAT News — December 20, 2019)
Solanezumab and the history of the future of treating Alzheimer’s disease (Forbes — November 11, 2016)
Hospitalized adults need their caregivers — they aren’t visitors (STAT News — March 29, 2020)
Continued bans on nursing home visitors are unhealthy and unethical (The Washington Post — July 13, 2020)
The long, exhausting reach of dementia care (STAT News - March 19, 2021)
Jason Karlawish’s Recommended Reads (Penn Memory Center — December 11, 2021)
A Case of Patient Abandonment, or an Abandonment of Patients? (The American Journal of Bioethics — June 23, 2022)
Advancing telemedicine beyond COVID-19 is the beginning of a revolution in dementia care (The Hill — August 27, 2022)
Don’t be so quick to blame aches and pains on getting older, two Philly doctors say (The Philadelphia Inquirer — October 19, 2022)
Clinical Practice in the Alzheimer Biomarker Era—Drugs for the Brain and Care for the Mind (JAMA Neurology — January 13, 2023)
Do people want to live longer with Alzheimer’s? (The Wall Street Journal — Dec. 14, 2023)
What the speculation about Joe Biden’s health can teach us about aging (The Philadelphia Inquirer — September 3, 2024)
Dementia risk, higher than thought, requires a national strategy (STAT — January 18, 2025)
How do persons with dementia suffer? (The Cambridge Quarterly of Healthcare Ethics - February 20, 2025)
Cuts to Medicaid will set the U.S. back 35 years in dementia care (STAT – March 25, 2025)
A Short Story Changed How I Care for Persons Living with Dementia (Journal of the American Geriatrics Society — 1 April 2025)
Why at-home Alzheimer’s tests may do more harm than good (The Philadelphia Inquirer — 12 November 2025)
Writings on decisional capacity:
Measuring decision-making capacity in cognitively impaired individuals (Neurosignals — December 5, 2007)
Assessing the Capacity to Make Everyday Decisions: A Guide for Clinicians and an Agenda for Future Research (American Journal of Geriatric Psychiatry — February 2008)
Everyday Decision-making Ability in Older Persons with Cognitive Impairment (The American Journal of Geriatric Psychiatry — August 21, 2009)
Is Harper Lee killing her own mockingbird? (The Philadelphia Inquirer — April 5, 2015)
Britney Spears Didn’t Feel Like She Could Live ‘a Full Life.’ There’s Another Way. (The New York Times — April 3, 2023)
Lucidity in persons with dementia
Once upon a time, I cared little about reports of (paradoxical) lucidity in persons with dementia, and then in June 2017, the NIA invited me to a small two day conference on the topic. Slowly, but then all at once, I began to change. I decided, this is something I need to pay attention to. (Paradoxical) lucidity describes an episode of connected communication in a person who has been thought to have lost that aspect of consciousness. I place the word “paradoxical” within parentheses because of what that word means. Something is “paradoxical” because it doesn’t conform to a theory. Here, the theory is persons with advanced dementia have lost their capacity for meaningful communication. A paradox is an aberrancy that ought to be dismissed. But what if episodes of lucidity were part of the experience of advanced dementia? Well, they wouldn’t be paradoxical. Research will answer that question. With funding from the NIA, my colleagues and I are deep into a study of the minds of persons with dementia.
Paradoxical lucidity: A potential paradigm shift for the neurobiology and treatment of severe dementias (Alzheimer’s and Dementia — August 2019)
Translating the discovery of covert consciousness into clinical practice (JAMA Neurology — March 16, 2020)
Sparks of Clarity (Penn Medicine Listening Lab — March 19, 2021)
What is paradoxical lucidity? The answer begins with its definition. (Alzheimer’s and Dementia — August 2, 2021)
The ethical implications of paradoxical lucidity in persons with dementia (Journal of the American Geriatrics Society — October 10, 2021)
Whealthcare
A person living with dementia is, to one degree or another, disabled. She’s developed problems performing her routine activities of daily living. Someone (or perhaps some robot or other clever device) needs to assist her to assure she has reasonable accommodations. There are many activities of daily living — preparing a meal, taking medications, traveling from one place to another, and so on. Through these activities, we express ourselves. We pursue what we desire. We enjoy what we like. This is the essence of that over used, perhaps abused, term “quality of life.”
For persons living with dementia, one of these activities stands out: managing finances. Problems managing finances are among the earliest signs of disabling cognitive impairments, and these problems can cause notable harms that include being a victim of abuse or exploitation, and costly mistakes.
Whealthcare isn’t just a clever play on words. In a word, this neologism assembles a truth. Health and wealth are intertwined in a twisted circle of causes and effects. In free-market, liberal democracies such as the United States, the banking and financial services industry ought to be on the front lines of detecting cognitive impairments, monitoring them, and intervening to assist their aging clients. Whealthcare challenges society not simply to think outside the metaphorical box, but to build new boxes, or something else entirely.
Whealthcare: Preventing Financial Fraud And Promoting Cognitive Health And Wealth (Forbes — June 4, 2016)
Spend Some Money To Make Money, Or The Opportunities Of Whealthcare (Forbes — January 27, 2018)
How bankers and doctors can collaborate to detect ‘early warnings’ of Alzheimer’s (STAT News — December 12, 2019)
Desktop Medicine and the Practice of Wealth Care (JAMA Network — November 30, 2020)
Advancing telemedicine beyond COVID-19 is the beginning of a revolution in dementia care (The Hill — August 27, 2022)
Importance of Asking Older Adults Whether They Are Having Difficulty Managing Finances (JAMA Open Network – September 13, 2022)
Voting Rights
To maintain and make more perfect our union, we the people vote. The act of voting is perhaps among the most essential expressions of self-determination and being counted as person. Sadly, since the beginnings of the United States, the right to vote has been a contested right. Just 100 years have passed since women were allowed the right. Even today, it remains contested. The voting rights of persons who live in long-term care facilities, and particularly those living with cognitive impairment, are easily ignored and consistently at risk. In a series of essays and studies, Karlawish has examined why and proposed and tested solutions.
Assisting Cognitively Impaired Individuals with Voting: A Quick Guide (available at American Bar Association Commission on Law and Aging)
Addressing the ethical, legal, and social issues raised by voting by persons with dementia (JAMA —September 15, 2004)
The Capacity to Vote of Persons with Alzheimer's Disease (American Journal of Psychiatry — 2005)
Policy statement on voting by persons with dementia residing in long-term care facilities (Alzheimer’s and Dementia — 2006)
Voting by elderly persons with cognitive impairment: Lessons from other democratic nations (McGeorge Law Review — September 2007)
Identifying the Barriers and Challenges to Voting by Residents in Nursing Homes and Assisted Living Settings (Journal of Aging and Social Policy — 2008)
Bringing the Vote to Residents of Long-Term Care Facilities: A Study of the Benefits and Challenges of Mobile Polling (Election Law Journal — 2011)
Older adults deserve to vote too — here’s the support they need (The Hill — October 22, 2020)
Desktop Medicine
In 2010, Karlawish published a short essay in the Journal of the American Medical Association, commonly known as JAMA. He argued something revolutionary is happening in medicine. Social forces, technologies and ways of thinking about numbers and risk have converged and changed how medicine and society think about what’s a disease and therefore who’s a patient and what care she’s owed. The space where these activities unfolded is transforming from the bedside of the sick patient to the desktop of the person at risk.
He coined the phrase “desktop medicine” to juxtapose this actuarial model of disease naming, diagnosis and treatment with the practice of “bedside medicine.” In that centuries-old practice, the patient’s narrative of his personal illness experience, often told while in bed because of illness, was the physician’s entre into diagnosis and treatment. The physician makes a diagnosis by matching the patient’s history of illness and findings from physical exam to the results of pathological studies of tissues. This practice is called “clinical pathological correlation.”
Desktop medicine replaces “clinical pathological correlation” with “clinical actuarial correlation.” Stethoscopes and reflex hammers are being replaced by fast networked computers, algorithms and biomarkers. The desktop doctor works like a kind of actuary who assesses a patient’s risks.
Hypertension, osteoporosis, diabetes. For these diseases, numbers rule how we think about our health. They offer the great promise of prevention but also the perils of prevention. We live at risk and are taken up in a vast private enterprise that effectively owns the genes, algorithms, drugs and biomarkers that define disease.
What about our desktop medicine for the diseases of the brain? The answers to that question reveal the opportunities and challenges of whealthcare and precision medicine for the brain.
Desktop Medicine (Journal of the American Medical Association — November 10, 2010)
Too Young to Die, Too Old to Worry (New York Times — September 20, 2014)
Statins by Numbers (New York Times — November 29, 2014)
Taking On The Challenges Of Precision Medicine For The Brain (Forbes — December 12, 2015)
My Amyloid Is 'Elevated' — So What's My Risk Of Getting Alzheimer's Disease? (Forbes — October 25, 2017)
Bio-Age Will Change Who We Are (And If We Have To Take Off Our Shoes At The Airport) (Forbes — May 18, 2018)